Radiotherapy after breast-conserving surgery for ductal carcinoma in situ reduces the risk of ipsilateral invasive recurrence but does not reduce breast cancer mortality, new research shows.
Analysis of data from 108,196 women diagnosed with ductal carcinoma in situ (DCIS), who were included in the Surveillance, Epidemiology, and End Results (SEER) 18 registries database, showed radiotherapy significantly reduced the risk of ipsilateral invasive recurrence at 10 years (adjusted hazard, 0.47; 95% confidence interval, 0.42-0.53; P less than .001) but only achieved a nonsignificant reduction in breast cancer mortality (adjusted HR, 0.81; 95% CI, 0.63-1.04; P = .10).
“The finding of greatest clinical importance was that prevention of ipsilateral invasive recurrence did not prevent death from breast cancer,” wrote Dr. Steven A. Narod and his colleagues from the Women’s College Hospital and the University of Toronto.
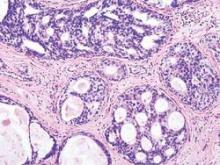
Though it is often stated that DCIS is a preinvasive neoplastic lesion that is not lethal in itself, these results suggest that this interpretation should be revisited, they said in the report, published online August 20 in JAMA Oncology.
“Some cases of DCIS have an inherent potential for distant metastatic spread. It is therefore appropriate to consider these as de facto breast cancers and not as preinvasive markers predictive of a subsequent invasive cancer,” they said.
The mean age at diagnosis of DCIS for the women in the database was 53.8 (range, 15-69) years, and the mean duration of follow-up was 7.5 (range, 0-23.9) years. Overall, the 20-year breast cancer–specific mortality rate following a diagnosis of DCIS was 3.3% (95% CI, 3.0%-3.6%).
Just over 1% of the 42,250 women treated with lumpectomy and radiotherapy developed an ipsilateral invasive recurrence in the follow-up period and 163 women (0.4%) died of breast cancer. Of the 19,762 women who were treated with lumpectomy without radiotherapy, 595 women (3%) developed an ipsilateral invasive recurrence and 102 women (0.5%) died of breast cancer, Dr. Narod and his associates reported (JAMA Oncology. 2015 Aug. 20 doi: 10.1001/jamaoncol.2015.2510).
Among the 956 women who died of breast cancer in the follow-up period, over half (517) did not experience an in-breast invasive recurrence prior to death. Of the 163 women who were treated with lumpectomy and radiotherapy and then died of breast cancer, 57.7% (94) did not experience an in-breast invasive recurrence prior to death. Among the 102 women treated with lumpectomy without radiotherapy who died of breast cancer, 51 did not experience an in-breast invasive recurrence prior to death (50.0%). Among the 154 women treated with a mastectomy (unilateral or bilateral) who died of breast cancer, 112 did not experience an in-breast invasive recurrence prior to death (72.7%), the investigators reported.
They found that young age at diagnosis and black ethnicity were predictors of breast cancer mortality. Young women diagnosed with ductal carcinoma in situ before the age of 35 years had a more than twofold greater risk of dying from breast cancer than older women (7.8% vs. 3.2%; HR 2.58, 95% CI, 1.85-3.60; P less than .001). Black women also had a much greater risk of dying from breast cancer than non-Hispanic whites (7.0% vs. 3.0%; HR, 2.55, 95% CI, 2.17-3.01; P less than .001).
“If DCIS were truly a (noninvasive) precursor of breast cancer, then a woman with DCIS should not die of breast cancer without first experiencing an invasive breast cancer (ipsilateral or contralateral), and the prevention of an invasive recurrence should prevent her death from breast cancer. Surprisingly, the majority of women with DCIS in the cohort who died of breast cancer did not experience an invasive in-breast recurrence (ipsilateral or contralateral) prior to death (54.1%),” the investigators said.
“The outcome of breast cancer mortality for DCIS patients is of importance in itself and potential treatments that affect mortality are deserving of study,” they concluded.
No relevant conflicts of interest were declared.